Why Claim Settlement Ratio is wrong parameter to look at?
Do you exactly understand what the Claim Settlement Ratio in Insurance is?
A lot of people just look at the claim settlement ratio and make an opinion about an insurance company. In this article, let me break some myths and help you understand more about the claim settlement ratio.
What is Claim Settlement Ratio?
In simple words, the claim settlement ratio is the percentage of claims paid in a financial year.
Claim Settlement Ratio = (No of Claim Paid / No of Claims Received)
So if a company gets 1000 claims in a year and pays 985 of them, then its claim settlement ratio for that year will be 98.5%. An important point to note here is that it’s about the number of claims and not the number of claims.
What type of Claims is considered in the Claim Settlement Ratio?
Generally, most of the people willing to buy a term plan look for this ratio as they are concerned about the claim getting paid in case of their early death. But claim settlement ratio is not the same as the “death claim settlement ratio”
In the calculation of the claim settlement ratio (in the case of life insurers), all types of claims are considered like.
- Death Claim: The claims once the policyholder dies
- Maturity Claims: Policies that are maturing and needs to be settled
- Surrender Claims: Policies that are closed prematurely and surrendered
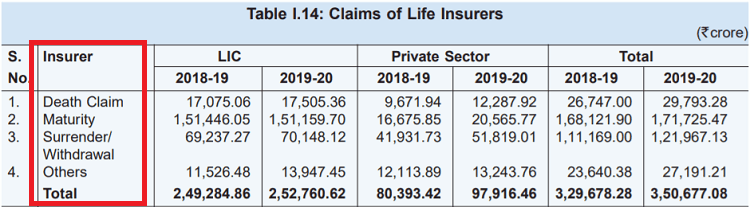
Here is the breakup from the IRDA report of 2019-2020, where you can see the number of claims for LIC and private insurers
Is Claim Settlement Ratio a probability?
One of the biggest myths about CSR (Claim settlement ratio) is that it’s a probability of claim settlement. This is not true and often leads to misjudgment of an insurance company.
CSR is simply a way of representing the data and nothing else. It does not tell you about the intention of the company. Let me share this with an analogy
Imagine there are two VISA processing counters which are looking at documents of people and giving the VISA or rejecting it.
Now if the Visa will be approved or rejected depends mainly on how proper are the documents and the person and not depend on the person who is processing the Visa. If the documents and case fall into the rules set, then it will be approved, else it will not.
So imagine there are two counters A and B . Counter A rejects 5 people out of 100 and Counter B rejects 7 people out of 100.
Now, this simply means that counter A got 5 people who did not fit into the set rules or their documents had issues. In the same way counter, B got 7 people who had incomplete documents.
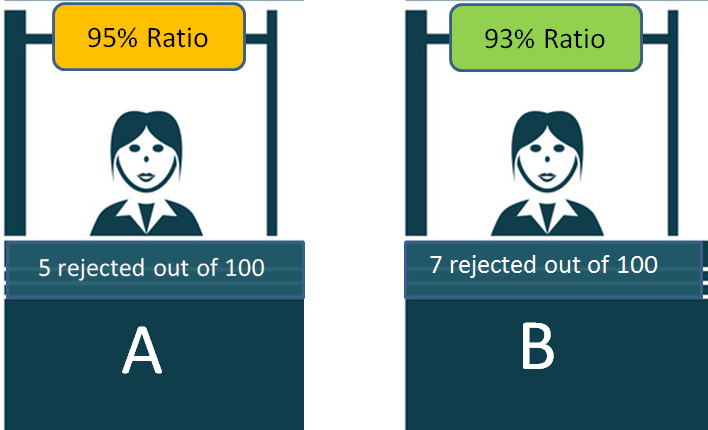
One cannot mistake these 93% (A) and 95% (B) as the probability of their visa getting rejected.
Hence, in the same way, the claim settlement ratio just tells you about what kind of claims did the insurance company received and how many of those claims were rejected. It’s not a probability.
Investors mostly have a very bad view of companies and attribute these rejections to their intentions, which is not a correct way to look at this ratio.
Does Claim Settlement Ratio depend on the policyholder?
Yes
A claim that will be rejected or accepted depends mostly on the policyholder itself. There are many people who file a claim which is bound to get rejected as it’s not valid as per the terms and conditions of the policy document.
Many policyholders also have a very vague and wrong impression of what is covered and what is not. They file claims based on flimsy assumptions and for things that are out of the scope of rules.
Let me give you an example.
Imagine a person who lied to the company while taking a term/health insurance, that he is a smoker and also went through some surgery in past. He lied to the company.
After some years the claim was filed (person died or got hospitalized) and now the company finds out the information provided by the insured person was false and hence the claim should not be paid in this case and it’s totally valid rejection.
So here it’s not the company who had the wrong intention but the customer who created a situation that led to claim rejection. Most of the policies which are rejected fall into this category.
From your end, you have to understand one thing. If you have bought your policy properly and revealed all the information properly, your claim will not be rejected. However, if you give reasons for the company to reject your claims, it will surely be rejected and there is nothing wrong with that.
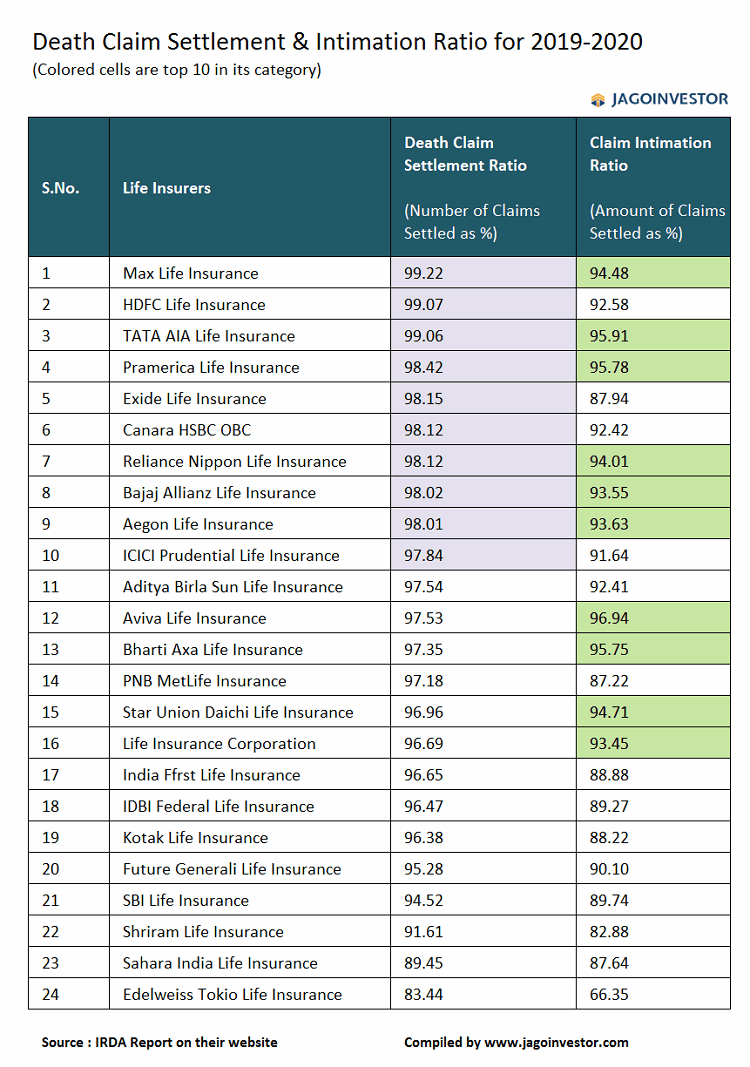
What is Claim Intimation Ratio?
Claim Settlement Ratio tells you about “number of policies”, whereas Claim Intimation Ratio tells you about the “AMOUNT”
It tells you what percentage of the claim amount was paid out of the total claim amount which was claimed in a year.
Claim Intimation Ratio = (Amount Paid / Total Claim Amount)
Most people are not aware of this ratio, and this gives you better clarity about the claims paid by a company. It may happen that a company has a high claim settlement ratio, but its claim intimation ratio is lower than the other company.
Here is an example of how the Claim settlement ratio can be high despite a low intimation ratio
Company A and B receives 10 claims in a year as follows
- 9 claims of Rs 10 lacs each
- 1 claim of 1.1 crore
[su_table responsive=”yes”]
| Company A | Company B | |
|---|---|---|
| Claim Rejected | 1 claim of 1.1 crores is rejected | 2 claims of 10 lacs are rejected |
| Claim Settlement Ratio | 9/10 = 90% | 8/10 = 80% |
| Claim Intimation Ratio | 90 lacs / 2 crores = 45% | 1.8 crore / 2 crore = 90% |
| Comment | Claim settlement ratio is high, but not the amount paid | Claim settlement ratio is low, but the higher amount paid |
[/su_table]
Business Model of an insurance company
As a customer, you should be very clear about the business model of an insurance company. An insurance company is a for-profit organization whose intention is to stay profitable and work for its profitability and also serve its customers as well.
The insurance company collects a small premium from a large number of people, but that money eventually goes only to a handful number of people who file for a claim. So in a way, it’s a shared resource which is given to those who are valid claimants.
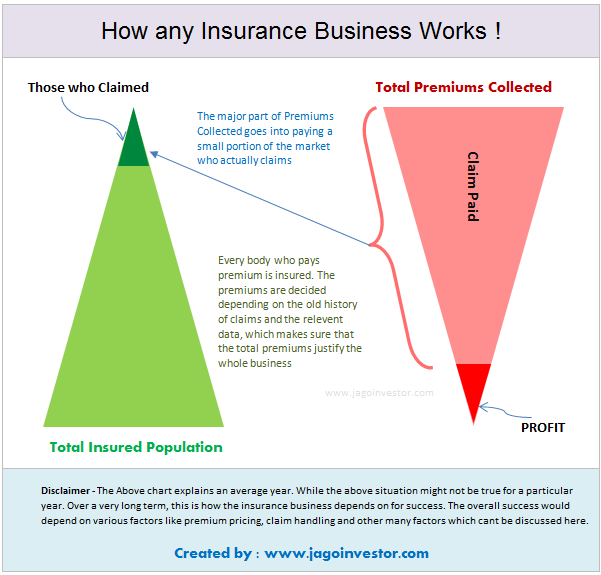
In order to stay in business and be profitable, an insurance company has to reject all the claims which are not valid. If they start paying each and every claim without proper verification, they just won’t survive and it’s not in the customer’s interest.
This simply means that a company with not the best claim settlement ratio, in reality, is a good company because knows how to protect itself and not let a fraudster make a wrong claim.
A very important point to note is that a new insurance company will mostly be getting death claims in the starting 8-10 yrs and not any maturity claims which means their claim settlement ratio may look on the lower side.
How to buy an insurance policy?
Basically here is a high-level step by step process
- Look at a company whose name you trust
- Choose a company which has been few years old (this depends on you)
- Choose a company whose product you like (features etc)
- Check out the experience of other investors online about the company
- Buy a policy with full honesty and by disclosing all information
Don’t lose your sleep over Claim Settlement Ratio
In the end, I just want to say that the claim settlement ratio is not a useful metric for any purpose and you should not lose your sleep over it. Don’t worry too much.
 May 18, 2021
May 18, 2021 
Manish ji thank you for the good article.
One question about claim settlement.
If someone quoted non smoker and takes a term insurance but let’s say the person starts smoking later or has been smoking already.
If death is not due to smoking, let’s say death is due to kidney failure or due to heart problem, can claim also be rejected?
Yes claim can still be rejected as in enquiry it is found to be a breach of trust. Also the death due to heart problem or kidney may somwhere be related to smoking !.. .who knows
Note that at the time of buying you have to be truthful
If one was not a smoker, they have to say they are a non-smoker “at the time of buying” .. Later they can start smoking, thats ok
Manish
Please review “Income plans till 99” e.g IndiaFirst Life Long Guaranteed Income Plan.
Are these really worth to go for ?
Avoid
ManishJi, As usual, its a fantastic article on selection of Life Insurance Policies.. Nicely explained for understanding for common people. I am definitely going to forward this to my friends..
Thanks
My agent says that a Diabetes (type2) and BP patient without any hospitalisaton history cannot make a claim within 4 years of purchase of policy for related to their preexisting diseases.
Diseases will be known only after admission into the hospital and if the patient is told that you will not be eligible for cashless or reimbursement treatment in the hospital.
Is there is anyway to know likely diseases from the above two pre existing diseases and organise funds for treatment
Note that insurance is for UNKNOWN SURPRISE EXPENSES in future.. Its not a way of arrangement of money!
Manish
Health Insurance or any insurance is for future UNKNOWN Surprise expenses. If someone already has it or has a hint that its going to come, insurance will not be provided.
Manish
Is this rule correct ?
I understand that if we pay premium for 3 continues years, no matter what information disclosed the claim should be paid to the nominee.
Clarity of 3 years insurance premium payment rule.
https://economictimes.indiatimes.com/wealth/insure/how-the-3-year-clause-impacts-life-insurance-claims/articleshow/66653173.cms?from=mdr
I think this is true in case of Term insurance. For health insurance, its 8 years. Pay premium for straight 8 years and claim cant be rejected as per IRDA. Unless it is in exclusion
Very useful information. It helps to understand that the policy buyer should look at Claim Intimation Ratio as an important metric rather than Claim Settlement Ratio.
Thank you Jagoinvestor for writing such helpful blogs!
Thanks a lot !
The information provided is indeed useful
I would request to provide article on categorization information of the companies as shown in figure (24 companies) on the basis of
i) Claim Settlement Ratio
ii) Claim Intimation Ratio
in regard to different types of claims separately like death claims, medi-claims, maturity, accidental as per riders applied, etc.. Also, it can on types of policies as well just like term insurance, endowment, moneyback, ULIP, Medical Insurance, Pension Products, etc.
Further, the way how can we request for such type data from company as well.
I feel then only we can get better picture for selection of company. Rest as what u say..
That data is not available at all!
As a consumer don’t you think IRDA should ask all insurance companies to make this data available?
Insurance companies do lack in trust from their side as well.
That data must be there with IRDA may be.. That data is just not into IRDA reports!
Though your query seems reasonable, all companies try to keep information guarded. Even in Annual results, they share the information that is mandated by MCA and no more. However, consumer activism is increasing and regulators and consumers are demanding more info. Slowly it may follow.
May be you can add below information also regarding life insurance policy, in the above article:
Insurance companies cannot reject claims made on policies over three years. According to the Insurance Laws (Amendment) Act 2015 Section 45 no claim can be repudiated (rejected) after 3 years of the policy being in force even if the fraud is detected.
Yea I can .. but the context is different here..
You mention this “After some years the claim was filed (person died or got hospitalized) and now company finds out the information provided by the insured person was false and hence the claim should not be paid in this case and its totally valid rejection”
Though all your points are valid , an additional point in above para will help.
‘In above case term insurance can only be rejected if claim is made within 3 years if information provided was false’
Yea .. Thats a good point to add.
I have first hand account of 4 different medical insurance claims (2 for my mother, 1 for an uncle and 1 for neighbor) . In all 4 of them insurance company was informed in advance and all documents submitted. But while discharging, they delayed approving the claim for flimsy reasons. Their tactic was to ask one question, when hospital responds to them (after usually 2-4 hours), they ask another unrelated question. This was frustrating and in 2 cases it went till late night. I had to call my company finance folks to call our insurance contacts to sort it out. Note that finally in all 4 cases, they paid, but they did their bit to frustrate you and hoped that you forget the claim. If I had not proceeded in any one, this would not have got counted in “number of claims received” as officially we did not respond and hence did not submit claim form fully. Now I have stopped paying premium and will use my own money for any expenses.
Thanks for sharing your experience. The company in our experience will make all attempts to make sure that the investigation is done fully. In health insurance, its not as simple as it sounds like life insurance where the chances of debate is NIL
Claim settlement ratio in Mediclaim is not calculated in the above manner. This is very misleading in Mediclaim.
The correct way should be No of Claims Paid divided by No of Claims received. I am talking of Mediclaim only.
Hi Ashit
Did I say anything different?
In the article its written Claim Settlement Ratio = (No of Claim Paid / No of Claims Received)
How to know what types of diseases occurring for a Type 2 Diabetes patient or a BP patient for over decades but never got hospitalised excepting for Cataract surgery ( Day treatment as out patient) will not be approved during the first 3-5 years of policy
Both the patients have no knowledge about what will happen if they get hospitalised for treatment.
Your question is not clear to me. Please rephrase the question
Really useful information
Thanks